Right now, around 2,000 people in England with learning disabilities and/or autistic people are living in ‘long-stay’ secure hospitals, often for many years and with no planned date for them to leave -despite repeated policies meant to help them live in the community. Researchers at Birmingham, led by Professor of Health and Social Care Jon Glasby, are asking what we can do to help them leave hospital and lead more ordinary lives...
Stuck in the system
Two years: that is the average time some people with learning disabilities and/or autistic people spend with their lives on hold in hospitals and inpatient units; and a few up to ten years. This is despite policy and press attention over recent care abuse scandals bringing these settings into the spotlight.

The problem is that not enough people seem to be listening.
Services are struggling to prevent people reaching crisis point in the first place, and to adequately support them in units a long way from friends and families. Despite the cost and inadequacies of the services, there has been surprisingly little research on why people get stuck in such settings, and little public awareness of the issue.
Why isn't this getting fixed? A report with a difference...
Jon's research team is working with the rights-based organisation Changing our Lives, finding out what the main barriers are, and what would genuinely help people to leave hospital. He explains: 'Previous research has often failed to talk directly to people with learning disabilities and/or autistic people, their families and frontline staff about their experiences of living or working in such settings, what they see as the main barriers and what would help more people to leave hospital. For us, failing to take into account their lived experience was not only morally wrong, but is wasting a major source of expertise with which to improve services.'
 Jon believes we already have the answers at our fingertips: 'People in long-stay hospitals know what kind of life they want to lead; they know that no one should "live" in a hospital and they often know what would help them leave – the problem is that not enough people seem to be listening.'
Jon believes we already have the answers at our fingertips: 'People in long-stay hospitals know what kind of life they want to lead; they know that no one should "live" in a hospital and they often know what would help them leave – the problem is that not enough people seem to be listening.'
Helping to transform services
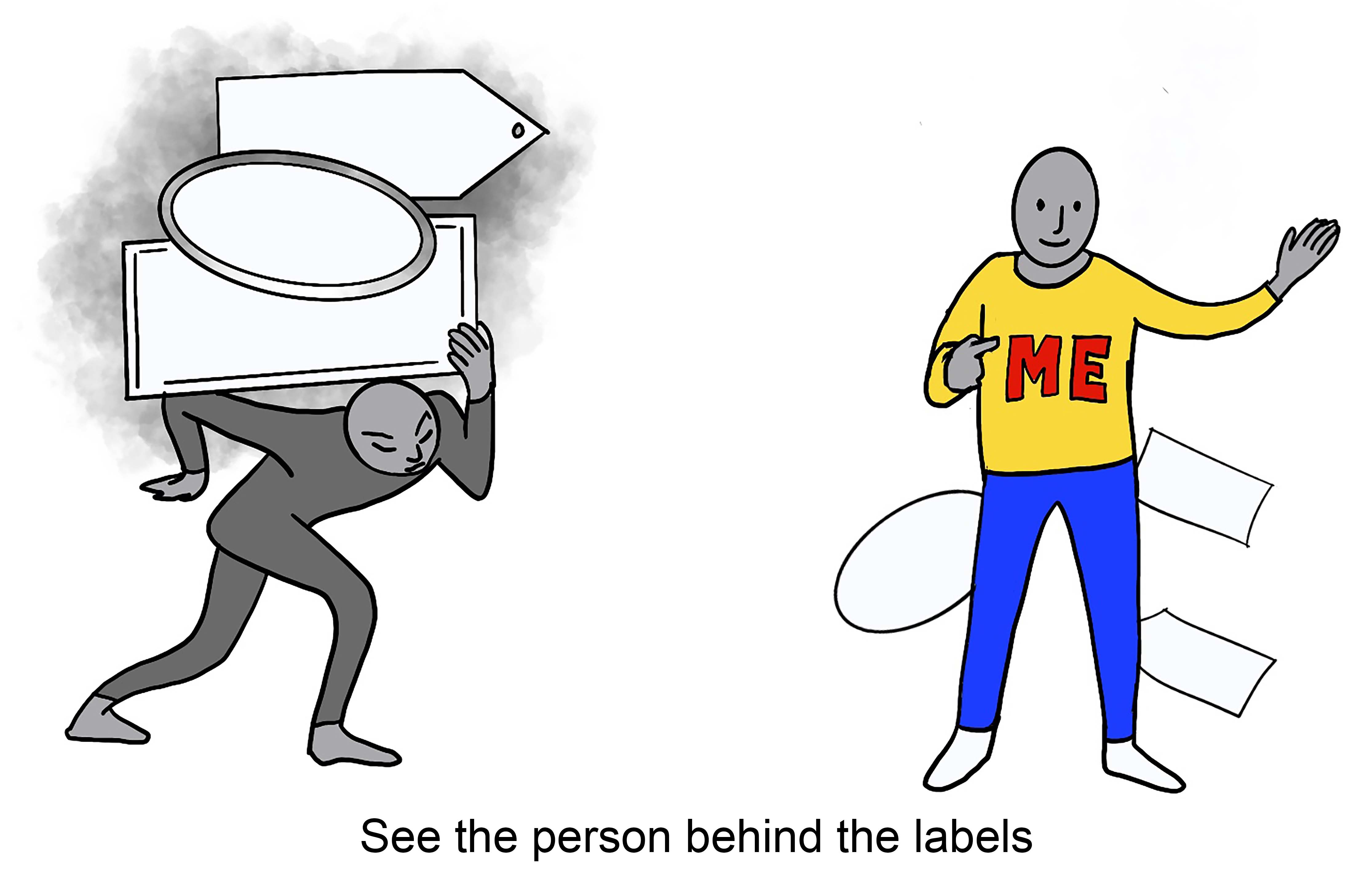
The report captured experiences to create 'ten top tips' (see images in this article) that have been shared with every health and social care leader in the country, including a free training video for care staff and an accessible version for people with learning disabilities. The topic will be looked at further through IMPACT, the new UK centre for implementing evidence in adult social care.
I feel like I'm going round and round in circles...(you) get so far and then hit a barrier'.
The University of Birmingham is the lead partner for IMPACT, funded by a £15 million ESRC and Health Foundation grant and drawing on insights from research, lived experience, and practice knowledge to make a difference to front-line services, and to people's lives.
The street artist amplifying patients' voices
The research found an unexpected ally in Birmingham-based artist, Foka Wolf, best known for his "subvertisements"; parodies of corporate and political posters.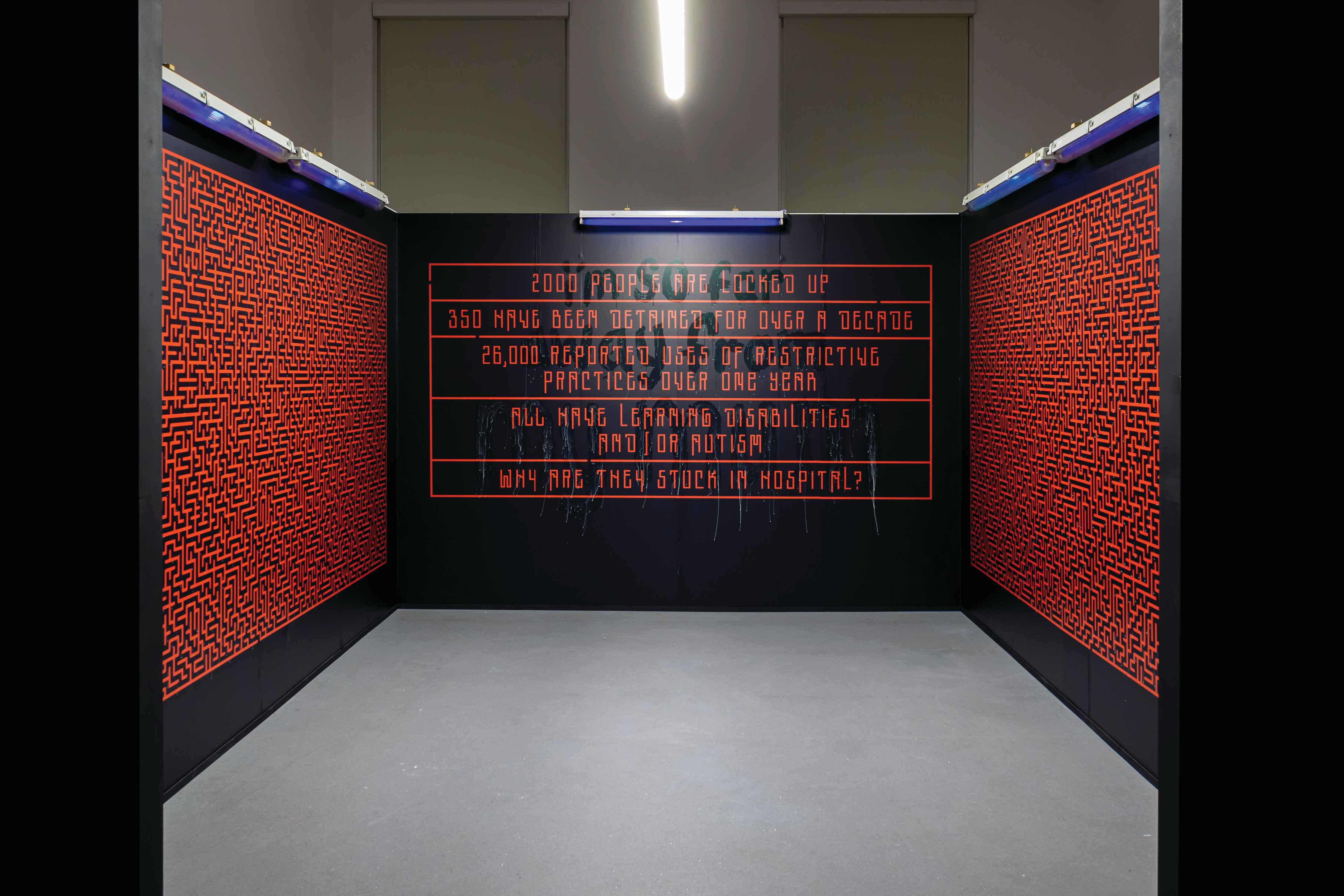
He lent his skills to bring to life the frustration and loneliness people feel, creating an art installation of an impossible maze filled with the words of those stuck in hospital: 'I'm so far away from my mum.'
'When I was told some of the stories about people trapped in social care I was gobsmacked,' says Foka on his involvement with the project.
'I felt naive for not knowing about any of this. The exhibition is less about the art and more about the message… and this is the perfect opportunity to tell people about it.'